17
to abrasive wear of the opposing dentition. For this reason, it has
been recommended to polish the occlusal surface of the zirconia
prior to glazing it. This would maintain the smooth surface in spite
of thewear of the glass-containing glaze layer. The opposing opinion
holds that even if the surface of the zirconia is polished, it will also
wear, resulting in the same surface profile as if the glaze was applied
and degraded during function. Current laboratory studies reveal
that polished zirconia is wear-compatible with the opposing denti-
tion similar to the glazed zirconia. Sintered, unpolished zirconia is
the most abrasive to the opposing dentition. A second aspect of this
discussion is concerning adjustment of the crowns post-cementa-
tion. Any adjustment to the surface of the zirconia must be repol-
ished to return the smooth surface to the restoration. Failure to do
so may result in abrasive wear of the opposing dentition. Most of
the evidence for the wear caused by zirconia is a result of laboratory
studies with simulated occlusal function systems. Clinical research
is needed to determine the clinical significance of this concept.
ESTHETICS
Zirconia is not as translucent as glass-containing ceramics and will
mask underlying tooth discoloration very well. This is a consid-
eration when trying to match the esthetic appearance of anterior
teeth, as zirconia will not exhibit the chameleon effect of absorbing
surrounding tooth color as well as more translucent glass-ceramic
restorations. The increased zirconia opacity also lends a brighter
appearance to the zirconia crown. It can be somewhat problematic
to decrease the value of the crown with surface stains and glaze.
And the increased opacity of the zirconia also prevents the cement
color from influencing the final shade of the crown.
ADHESIVE BONDING OF ZIRCONIA
Increased surface roughness provides a more extensive area for
adhesion. Zirconia is polycrystalline and does not contain glass.
This is significant because etching glass is the process by which
glass-containing ceramics are adhesively bonded to the tooth.
Therefore, this is not an option for zirconia restorations.
Some reactive agent needs to be imparted to the surface of the
zirconia to have the potential for adhesive bonding. A hydrophobic
phosphate monomer, 10-methacryloyloxydecyl dihydrogen phos-
phate (10-MDP) has reported ability to bond to zirconia. Air abrasion
with silica acidmodified alumina (CoJet Sand) and the application of
anMDP-containingbonding/silane couplingagentmixture increases
the bond strength between zirconia and resin cements. Although a
degree of adhesion is possible with zirconia, cementation with resin-
modified glass ionomer cements (RMGIC) is generally preferred as it
is amore efficient clinical technique with easier clean-up.
The strength of zirconia and opportunity to cement rather than
bond zirconia crowns requires more mechanically retentive tooth
preparations compared to thoseadvocated for adhesiveceramic resto-
rations. Acementedcrownrequires at least 3.0mmof clinical prepara-
tion height to resist dislodgement. The degree to which an adhesive
cement for zirconia crowns with less than 3.0mmpreparation height
may ensure adequate resistance to dislodgement is unknown.
CONCLUSION
The tooth preparation will be a more significant influence on the
risk of crown dislodgement compared to adhesively bonded glass
ceramics since RMGIC will contribute little to adhesive retention
of the crown. The surface hardness of zirconia will emphasize the
need for accurate design of crown contours and contacts to avoid, or
at least minimize, the need for post-sintering adjustment and repol-
ishing. And the brighter, less translucent appearance of zirconiawill
have an impact on the esthetic application of full contour zirconia
crowns in the anterior dentition.
The high strength of full-contour zirconia is a desirable feature, as it
prevents themost common failureof glass ceramics: chippingand frac-
ture. This may be an advantage in high-stress clinical situations with
potentially limited interarch space to create the 1.5mmocclusal reduc-
tionrequired for glass ceramic restorations. Theopportunity tocement
with aRMGIC is obviously an advantage in clinical ease and efficiency.
Chairside full-contour zirconia crowns will afford many clinicians a
very strong, fracture-resistant alternative restorativematerial.
For questions and more information, Dr. Fasbinder can be reached
at
.
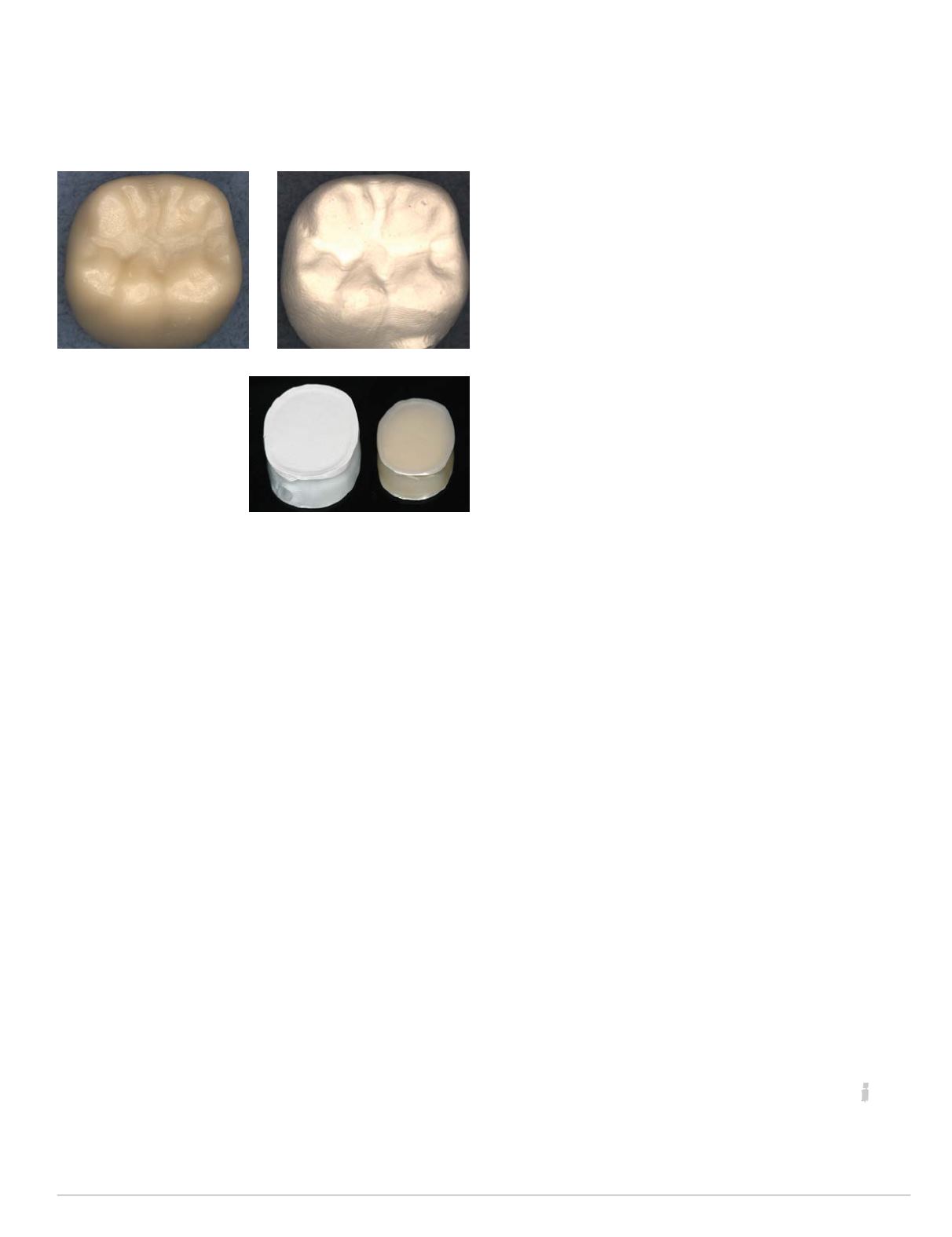
Sirona TZI-C sintered
crown (above); standard
milled pre-sintered
restoration (top right);
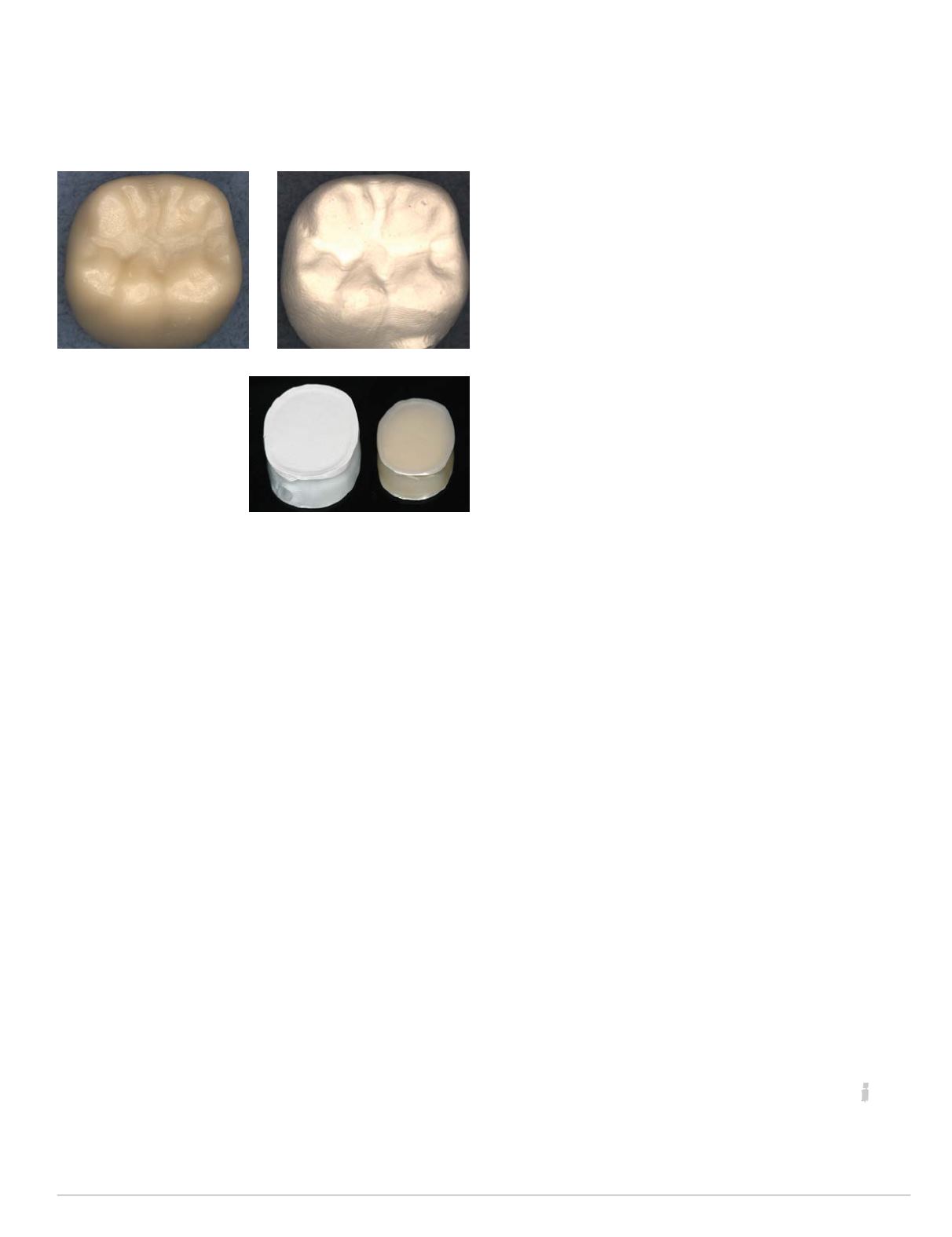
Zirconia disc size
comparison (right)